More than 360,000 Service members have suffered traumatic brain injuries (TBI) since 2000, according to the Defense and Veterans Brain Injury Center (DVBIC). Active duty and reserve military men and women are at increased risk for sustaining such injuries partially because many routine operational and training activities are physically demanding and even potentially dangerous. In addition, Service members are deployed to areas where they are at risk for experiencing blast exposures from improvised explosive devices (IEDs), suicide bombers, land mines, mortar rounds and rocket-propelled grenades.
Although recent attention has intensively focused on combat-related TBI, DVBIC notes that TBI can occur during normal daily activities outside of official duties. Service members enjoy challenging leisure activities like motorcycle riding, mountain climbing, skydiving, hunting, sailing and rappelling, to name a few. In addition, an integral part of active duty military life is physical training, which can include martial arts, running, weight lifting and intensive physical conditioning. While these activities contribute to a positive quality of life, they also increase risk for TBI.
TBI can be classified as mild (such as a concussion), moderate, severe or penetrating. Recovery is contingent on the severity of classification. For example, most people recover from a concussion while severe or penetrating TBI may cause long-term cognitive disability. Additionally, like all injuries, recovery is different for each individual.
According to David O. Okonkwo, MD, PhD and clinical director of the Brain Trauma Research Center of the University of Pittsburgh, no U.S. Food and Drug Administration (FDA)-approved pharmaceutical interventions are available for TBI and little consensus exists regarding effectiveness of cognitive rehabilitative strategies. “Due to the heterogeneous of these injuries, there is a strong need to develop protocols for identifying the specific problems and complications of individuals suffering from chronic TBI symptoms. This type of clinically actionable information could guide targeted therapies for patients, leading to improved cognitive function and decreased symptoms.”
To help address the growing need to support TBI research and treatment, Congress established the Department of Defense (DOD) Psychological Health and Traumatic Brain Injury Research Program (PH/TBIRP) in FY07. Original appropriations of $300M were assigned for “the purpose of soliciting and managing critical TBI-and PH-related research and development efforts to benefit Service members, veterans and other beneficiaries of the Military Health System. FY17 funding includes $850,000 “to overcome historical challenges associated with human subject recruitment by supporting research leveraging existing data from the Department of Defense Trauma Registry (DoDTR) to rapidly identify actionable insights into the management of TBI.”
According to Mount Sinai Professor Guilio M. Pasinetti, MD, PhD and member of the FY09 PH/TBI Research Program Peer Review Panel, mild TBI can be difficult to diagnose and, when coupled with psychological illness, either misdiagnosed or missed altogether. However, with the advent of genomics and proteomics technologies, personalized medicine offers the promise and potential for uncovering the largely “unseen” details of disease causality, onset and progression.
In his 2012 study, Pasinetti and fellow researchers sought to identify clinically accessible molecular biomarkers that could be used to help identify veterans suffering from effects of mild traumatic brain injury (mTBI). While analyzing the expression profile of small non-coding RNAs in peripheral blood mononuclear cells (PBMCs) from a veteran study cohort, the team identified 18 candidate small non-coding RNA biomarkers that are differentially regulated in PBMCs of mTBI compared to non-TBI control cases. Of these candidate small RNA biomarker species, 13 are significantly down-regulated in PBMCs of mTBI compared to non-TBI control veteran cases. Additionally, the team identified a 3-biomarker panel that was most able to distinguish mTBI from non-TBI control veteran cases with high accuracy, selectivity and specificity. By identifying clinically accessible molecular biomarkers of mTBI, doctors may now have an additional tool to broaden more traditional diagnostic practices.
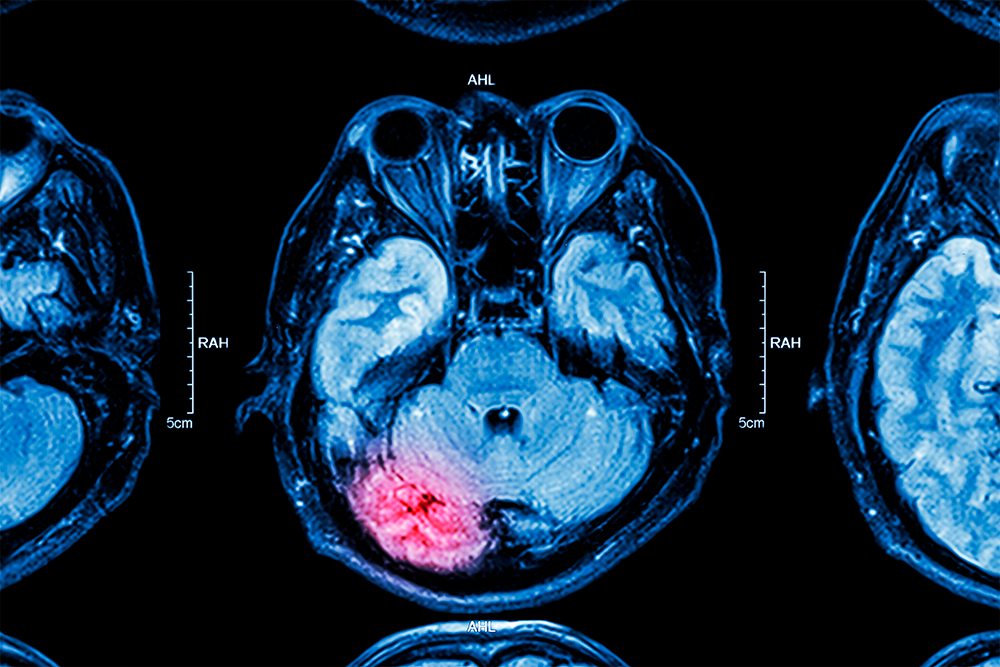
Standardized diagnosis of brain injury involves looking for signs of brain injury, either through CAT scans, MRIs and X-rays or through screening tools – usually in the form of simple tests – that measure various areas of a person’s speech, movement, memory and thought. Often tests used to diagnose injury help determine the appropriate course of treatment. For example, treatment for mTBI often involves resting the body and brain while treatment for moderate to severe injury usually focuses on medicines and surgical procedures. Once a person has been stabilized, treatment focuses more on recovery of lost abilities or learning to do things in a new way.
It is important to note that while 250,000 service members were diagnosed with TBI between January 1, 2002, and December 31, 2012, a total of 4,683 lives were lost. Kevlar body armor and helmets are cited for the reduced fatality to increased TBI ratio in wounded military. In her article, “Traumatic Brain Injury in the War Zone,” published in The New England Journal of Medicine (May 2005), Susan Okie, MD, notes that by “effectively shielding the wearer from bullets and shrapnel, the protective gear has improved overall survival rates, and Kevlar helmets have reduced the frequency of penetrating head injuries.” However, Okie points out that the helmets cannot completely protect the face, head and neck, and they do not prevent the kind of closed brain injuries often produced by larger blasts caused by an improvised explosive device (IED).
According to the 2012 Military Medicine article, “Mild Traumatic Brain Injury, Screening, Diagnosis and Treatment,” many initiatives have been implemented since 2006 to improve care for Service members with TBI, specifically mTBI. “Surveillance efforts aimed at identifying the incidence and prevalence of combat-related TBI have improved the availability of TBI-specific resources both in-theater and in-garrison. This is largely attributable to enhanced screening methods, which occur at various locations throughout the deployment cycle.
“Mandated Clinical Practice Guidelines (CPGs) standardize care and provide both evaluation and treatment recommendations to those on the battlefield as well as stateside. Opportunities for TBI education have expanded, now including regional/national conferences, online case studies, training modules and instruction at some deployment platforms. The evolution of telehealth capabilities allows providers the ability to treat injured service members in-theater, which may minimize the need for evacuation from theater or transfer to major military treatment facilities (MTF). Finally, ongoing research seeks to identify ways to mitigate blast exposure and effects, determine similarities/differences between blunt and blast TBI, and establish treatment paradigms to enhance TBI care.”
References:
- Select non-coding RNA in blood components provide novel clinically accessible biological surrogates for improved identification of traumatic brain injury in OEF/OIF veterans. Giulio M Pasinetti, Lap Ho, Christopher Dooley, Bhavna Abbi, Gudrun Lange. http://ajnd.us/files/AJND1204005.pdf
- Traumatic Brain Injury in the War Zone. Susan Okie, M.D, The New England Journal of Medicine, May 14, 2005. http://www.nejm.org/doi/full/10.1056/NEJMp058102#t=article
- Defense and Veterans Brain Injury Center (DVBIC). http://dvbic.dcoe.mil/tbi-military
